Several blood tests have been shown to diagnose with precision Alzheimer’s disease – As previously reported by Fox News Digital, but now a new test has emerged that can measure how far it has progressed.
The study, which was published on Monday in Nature Medicine Journal, was led by researchers at the University of Washington’s Faculty in St. Louis and the University of Lund in Sweden.
Determining the clinical stage of dementia can help ensure that the patient receives more beneficial treatmentAccording to the researchers.
Dementia related to Alzheimer’s could be avoided by the experimental medication, the researchers say.
The new test could also help confirm whether Alzheimer’s condition or another is causing a person’s symptoms.

According to researchers, a new blood test has emerged that can measure Alzheimer’s disease to progress. (Istock)
The researchers analyzed blood samples for 163 people who were experiencing several levels of cognitive impairment, from the presytomatic dementia to the early stage to the dementia in the late stage.
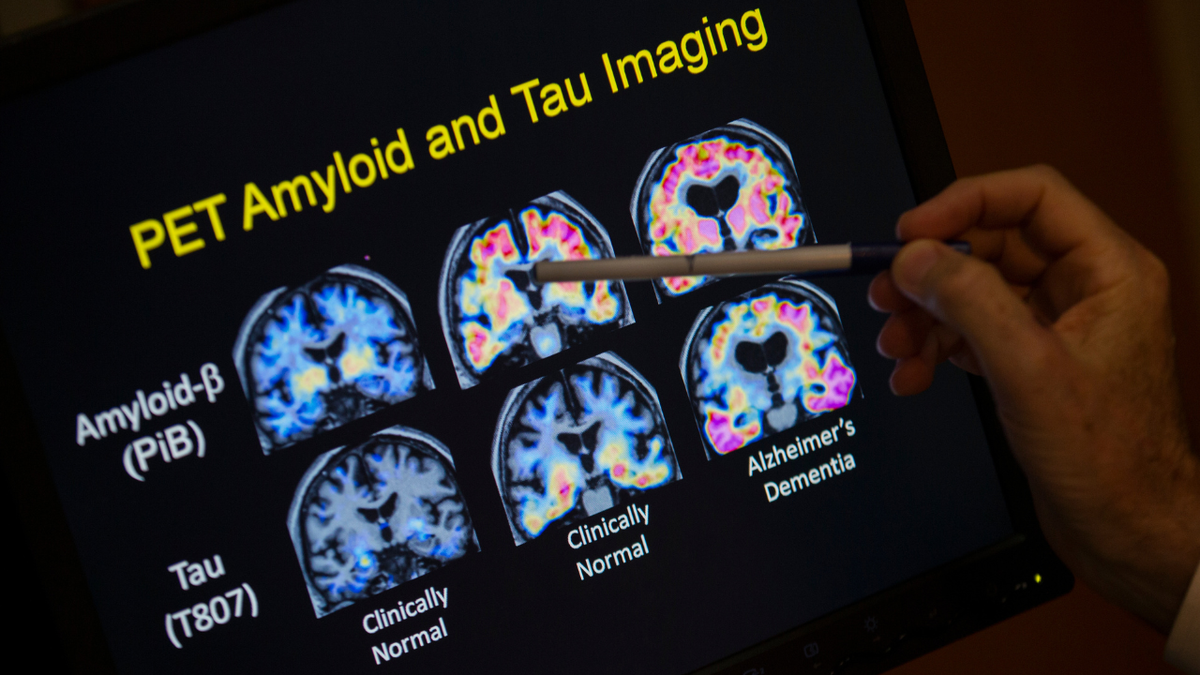
They discovered that the levels of a protein called MTBR-TAU243 correlate with the amount of Tau that has accumulated in the brain, according to a press release from Washu. The precision compared to brain scanning was 92%.
The largest amount of Tau accumulation, the more severe are the symptoms of Alzheimer’s.
MTBR-TAU243 levels were normal in people who still had no symptoms, indicating that protein is associated with more advanced stages.
The levels were also normal for people whose symptoms were linked to another cause that is not Alzheimer’s.
What to know about Tau
Tau is a protein that is grouped and “entangle” in the brain of people who have Alzheimer’s, health. These tangles interfere with cognitive function.
Tau tangles are generally formed years after the formation of another protein called amyloid, which creates plates in the brain and is one of Alzheimer’s first characteristics.
The higher the amount of Tau accumulation, the more serious are Alzheimer’s symptoms, it was 200 times greater for those in later dementia stages, according to the study.

PET brain scanns (positron emission tomography) are now the standard for staging, but they have some inconveniences, the researchers said. (Istock)
“The amyloid plaques and tau tau together define the basics Biological brain changes Of Alzheimer’s disease, along with the loss of brain cells and synapse, “Courtney Kloske, Ph.D., director of scientific participation of the Alzheimer’s Association in Chicago, told Fox News Digital.” These changes cause well -known memory and symptoms of dementia thought. “
While the blood tests developed previously measure the levels of amyloid plaques in the brain, this is the first to measure tau levels.
Two drugs from Alzheimer help patients to live independently at home for longer periods
“To help in early detection, we have seen advances in blood analysis, which have been shown to be very precise and are now available to help doctors in their diagnostic study,” Kloske said.
“The current study is analyzing the precision of a blood test for Tau; once these blood tests are developed, confirmed and validated, the positive results in both tests would strongly confirm Alzheimer’s disease as the cause of the person’s dementia. This makes a safer and definitive diagnosis and clarify Treatment options“

“This blood analysis clearly identifies the tau de Alzheimer’s tau, which is our best biomarker measure of symptoms and Alzheimer’s dementia,” said a researcher. (Istock)
The co-senior author Randall J. Bateman, MD, Charles F. and Joanne Knight distinguished neurology professor at Washu Medicine, pointed out that in Clinical practice Today, there is no easy or accessible measure of tangles and Alzheimer’s dementia.
“This blood test clearly identifies the tuo of Alzheimer’s tau, which is our best biomarker measure of the symptoms and dementia of Alzheimer’s,” he said in the statement.
“A blood test in Maraña such as this can provide much better indication if the symptoms are due to Alzheimer’s, and can also help doctors to decide which treatments are better for their patients.”
Looking to the future
The hope is that this new blood test can facilitate the creation of Alzheimer’s patients and adapt the treatments to their individual needs.
Click here to get the Fox News application
PET (positron emission tomography) brain scan They are now the standard for the staging, but they have some inconveniences, the researchers said.
They are “expensive, which require a lot of time and are often not available outside the main research centers”, which limits its use.
“For the early stages with tango low, anti-amyloid therapies could be more effective than in the late stages. But after the start of dementia with tangles of high Tau, anti-tau therapy or one of the many other experimental approaches may be more effective,” said a researcher. (AP Photo/Evan Vucci, Archive)
“We are about to enter the Age of Personalized Medicine for Alzheimer’s disease,” said the authors Kanta Horie, PhD, PHD, associate professor of neurology research at Washu Medicine, in the launch.
Click here to register in our health newsletter
“For the early stages with tango low, anti-amyloid therapies could be more effective than in the late stages. But after the start of dementia with tangles of Alta Tau, anti-tau therapy or one of the many other experimental approaches may be more effective,” he continued.
“Once we have a clinically available blood test for staging, plus treatments that work at different stages of the disease, doctors can optimize their treatment plans for the specific needs of each patient.”
“We are about to enter the Age of Personalized Medicine for Alzheimer’s disease.”
Kloske echoed the need for More research.
“While this research is promising for more early detection methods, we need to see the replication and expansion of these results in larger and more representative study populations to understand the implications in the general population,” he told Fox News Digital.
For more health articles, visit www.foxnews.com/health
The study was financed by the Charles F. disease research center and Joanne Knight Alzheimer, the Tracy Family Silq Center, the National Institutes of Health (NIH), the Zenith Award of the Alzheimer’s Association, the Hope Center for Neurological Disorders and the Department of Neurology of Washu Medicine.


